Antenatal Information
What is antenatal care?
This is the care you receive whilst you're pregnant to make sure you and your baby are as well as possible.
- I HAVE JUST FOUND OUT I AM PREGNANT
Click here to register your pregnancy.
Contact numbers for Community Midwives
Wigan South Team 01942 481487
Wigan North Team 01942 483602
Ashton Team 01942 482476/7
Leigh Team 01942 481198
Daisy Team 01942 822772
When will my baby be due?
Your official due date will be confirmed once you have had your first scan, if this is something that you choose. In the meantime, you can use the following NHS link to calculate your estimated due date https://www.nhs.uk/pregnancy/finding-out/due-date-calculator/.
Pregnancy and Multivitamins
https://www.nhs.uk/pregnancy/keeping-well/vitamins-supplements-and-nutrition/
- WHERE CAN I HAVE MY BABY?
You can choose to book your pregnancy and give birth at any Trust.
We hope that you choose WWL as we are a friendly team and will welcome you and your family. We can support you to birth your baby at home or on the Delivery Suite, where we also have a birthing pool.
Please see the links below for some further information about the choice of place of birth across Greater Manchester:
- WHERE WILL I HAVE MY ANTENATAL CARE IF I CHOOSE WWL?
You will see your named midwife in one of our clinics within our community settings. If you are required to attend an obstetric (doctor’s) appointment or a scan this will either be at the Thomas Linacre Centre (TLC) or Leigh Infirmary.
At most antenatal appointments you will be asked to have your blood pressure taken to check that it is within normal limits, as some women develop high blood pressure in pregnancy. Your midwife/obstetrician will also ask to test your urine to ensure that you have not developed a urine infection and/or protein in your urine which can be a sign of pre-eclampsia. Therefore, it is a good idea to always bring a sample with you.
https://www.nhs.uk/conditions/pre-eclampsia/.
At each attendance with a midwife you will also be asked to undertake a carbon monoxide screening test, this is to enable the midwives to offer support to those women who smoke or to identify if secondhand smoke is affecting you or if there could be a potential problem with your central heating system at home
We have the following specialist antenatal clinics:
Diabetes Clinic
Some women have type 1 or 2 diabetes before they become pregnant, whilst some other women are at risk of developing gestational diabetes (GDM) once they become pregnant.
These include: women with a BMI >30, certain ethnic minority groups, previous GDM, or a first degree relative with diabetes. If you are in this group you will be offered a blood test during your pregnancy at 26 – 28 weeks.
If you already have diabetes or are diagnosed during pregnancy your care will be overseen by the team of obstetricians and midwives in the Pregnancy Diabetes Clinic.
Please follow the link for information on gestational diabetes: https://www.nhs.uk/conditions/gestational-diabetes/.
Fetal Medicine
The Fetal Medicine Clinic is based at the Thomas Linacre Centre. Some women are referred here if there are any physical concerns seen on their ultrasound scan and their baby requires closer monitoring during pregnancy. You will be seen by an obstetrician specialising in fetal medicine and screening midwife.
Multiple Births
Once you discover that you are pregnant with more than one baby, you will be cared for by one of our obstetricians who has a specialist interest in multiple pregnancies. You will probably be asked to attend antenatal more regularly than if you were pregnant with a single baby.
https://twinstrust.org/let-us-help/pregnancy-and-birth.html
Rainbow Clinic
Since 2020 the Rainbow Clinic provides individualised care for women who have had:
- A previous miscarriage over 20 weeks gestation that was caused because of a problem with your cervix or the placenta
- Stillbirth
- Your baby died within 28 days of being born
Your care will be provided by the Bereavement Midwife and an obstetrician at the Thomas Linacre Centre (TLC).
Where to find the Antenatal Clinics
- PREGNANCY SCREENING INFORMATION
We would like to introduce ourselves as the screening co-ordination team for maternity at WWL. Our team consists of:
Janice Reid – Screening Midwife
Janet Barker – Screening Midwife
Joanne Clayton – Failsafe Officer
We are based at Thomas Linacre Centre and can be contacted on 01942 774702.
During your pregnancy you will be given many choices about what tests are available to you. These include, but are not limited to, blood tests, scans, and screening for abnormalities
Please follow the link below for further information, which also includes the option to read in a different language and to watch short videos.
https://www.gov.uk/government/publications/screening-tests-for-you-and-your-baby/introduction
Infectious Diseases – HIV, Hepatitis B and Syphilis
You will be advised to have screening blood tests to see whether you have had these infectious diseases in the past. This is because these infections can be passed to the baby during pregnancy or childbirth and you may not be aware that you have been infected. If any of them are positive there are measures that can be taken to prevent your baby becoming infected. There are also treatments that will help your own health.
https://www.gov.uk/government/publications/screening-tests-for-you-and-your-baby/infectious-diseases
Screening for Sickle Cell and Thalassaemia
Sickle cell anaemia and thalassaemia are inherited disorders that can cause anaemia. All women booking to deliver their baby at WWL will be offered screening for these disorders with a blood test. If you are found to be a carrier of the disorder, your partner will also be offered a test as parents who are both carriers have a one in four chance of having a baby with serious anaemia.
Screening Tests for Down’s, Edwards’ and Patau’s Syndrome
Down’s syndrome is a chromosomal disorder that affects around 1 in 1000 pregnancies and happens when the baby has an extra copy of chromosome 21. Children with Down’s syndrome have learning problems and sometimes physical complications.
You can read more about Down’s syndrome here: https://www.downs-syndrome.org.uk/
Edwards’ syndrome is a chromosomal disorder that affects around 3 in 10,000 births and happens when the baby has an extra copy of chromosome 18.
Patau’s syndrome is a chromosomal disorder that affects around 2 in 10,000 births and happens when the baby has an extra copy of chromosome 13.
Both of these conditions are serious and babies with these conditions have a range of physical and learning problems. Sadly the survival rates are low and of those babies born alive only around 13% with Edwards’ syndrome and 11% with Patau’s syndrome will live past their first birthday. Some babies may survive to adulthood but this is rare.
You can read more about Edward’s and Patau’s syndromes here: https://www.soft.org.uk/
Screening for these conditions is optional and the choice whether to accept screening or not is a very personal one. You may choose not to have screening for these conditions at all if you prefer.
The tests currently offered at WWL under the NHS screening programme are:
Combined screening (Nuchal Translucency (NT) scan and a blood test)
This is offered early in pregnancy between 11 weeks and 2 days and 14 weeks and 1 day. The test includes an NT scan which measures the amount of fluid at the back of your baby’s neck and a blood test which measures the level of two hormones in your blood. This information is combined with your age to estimate the chance of your baby having Down’s, Edwards’ and Patau’s syndrome. You can choose to have screening for Down’s syndrome alone, Edward’s and Patau’s syndromes only or for all three conditions.
Quadruple test (blood test)
This test is offered later in pregnancy between 14 weeks and 2 days and 20 weeks for those women who are too late for combined screening at their dating scan or for those where it was not possible to obtain the NT measurement. The test measures four hormones in your blood and combines this with your age to estimate the chance of your baby having Down’s syndrome. This test cannot give a result for Edward’s or Patau’s syndromes.
These tests cannot tell you whether your baby definitely has Down’s, Edwards’ or Patau’s syndrome. They simply tell you whether you have a higher chance (defined as a chance higher than 1 in 150) or lower chance of having a baby with Down’s, Edwards’ or Patau’s syndrome.
If the screening tests show that you are in the lower chance group you will usually receive a letter informing you of this within two to three weeks of the test.
If the screening test shows that you are in the higher chance group, the options for management will be discussed with you. This will include the offer of a further test of an amniocentesis or Chorionic Villus Sampling (CVS) to find out if your baby has Down’s, Edwards’ or Patau’s syndrome or not (these are over 99% accurate). These tests both have a risk of miscarriage of 1%.
More detailed information on these tests can be found in the STFYAYB booklet.
Non-invasive prenatal testing (NIPT)
This is a test developed in the private sector to screen for Down’s, Edward’s and Patau’s syndrome and is now available on the NHS for those women with a higher chance result from the combined or quad test. The test looks for DNA from the placenta in the mother's blood stream and the screening test result shows if there is a low chance or a high chance of your baby having Down's, Edward's or Patau's syndrome more accurately. If the result shows a high chance this would still need to be confirmed by an invasive test such as amniocentesis to be absolutely certain.
A number of private clinics continue to offer this service and the price varies from £350-£550 for those women who choose to have this test instead of a combined / quad test. More information and a list of local centres who offer this screening can be obtained from Antenatal Results and Choices on 0845 077 2290 https://www.arc-uk.org/.
Ultrasound scans
Dating scan
This scan is performed usually between 10 and 14 weeks to check your baby’s heartbeat, the number of babies and to calculate when your baby is due. Occasionally, a problem may be seen on the scan and if this is the case an appropriate review appointment will be arranged with either the screening midwife or a consultant specialist.
Structural (Anomaly) Scan
This scan is performed usually between 18 weeks and 20 weeks plus 6 days to check whether your baby is developing normally or whether it has any obvious abnormality. If there is a problem seen on the scan an appropriate review appointment will be arranged with either the screening midwife or a consultant specialist.
https://www.wwl.nhs.uk/media/.leaflets/602b91a97a0b56.14044868.pdf
- MENTAL HEALTH IN PREGNANCY
One in five women experience a mental health problem during pregnancy or in the postnatal period. Women can feel anxious or can feel depressed during this period and it is not uncommon to worry about:
- Upcoming changes to their life and how they might cope as a new parent
- Fear of childbirth
- Changes to existing relationships
- Lack of support and/or being alone
- Physical health and pregnancy problems
You are not alone and there is support available to you please speak to your GP and/or midwife.
If you feel suicidal please go to your nearest Emergency Department (A&E).
https://www.nhs.uk/pregnancy/keeping-well/mental-health/
https://www.rcpsych.ac.uk/mental-health/treatments-and-wellbeing/mental-health-in-pregnancy
Specialist Mental Health Midwife Service
We have a small team of Specialist Perinatal Mental Health Midwives at Wigan, Wrightington and Leigh NHS trust. Lyndsey Banks and Nicola Bolton
They can be part of your care during your journey through pregnancy and into parenthood if your current or previous mental health difficulties are identified as moderate/severe or complex by your midwife.
They work alongside our established Community Midwife Service, Daisy Team Midwives’, and hospital midwives to meet the needs of every woman and their families effected by mental health in pregnancy and beyond.
They work closely with the Specialist Perinatal Mental Health service and other emotional wellbeing services, along with your maternity team, health visitor and GP ensuring a family is offered the best support in their pregnancy and following birth to develop their self-confidence, support bonding and address a woman’s needs and wishes for the future with her baby. It is their role to ensure that you are provided with compassionate, non-judgemental supportive care, to empower you to make your own decisions.
Together, they can discuss your preferences for care around pregnancy and birth and will promote your relationship with your baby, and provide you with additional information about how your mental health and medication can impact on your pregnancy and breastfeeding. The service also enables women experiencing previous trauma, birth trauma or birth fear, the option of a holistic plan of care to address women’s worries and fears around their birth experience.
Some women will also be offered a specific mental health plan of care that outlines when in hospital how we support their individual needs, this could be around who they wish to be at the birth, medication and breast-feeding advice, and support and follow up for women and their babies once home.
The team are available as a resource for other professionals with regards to perinatal mental health to support women to access the most appropriate care / service to meet their needs.
- PERINATAL WELL BEING COURSE
- VACCINATIONS IN PREGNANCY INCLUDING COVID-19
Please follow the links below for further information on vaccinations:
Pregnancy: how to help protect you and your baby - GOV.UK (www.gov.uk)
https://www.nhs.uk/pregnancy/keeping-well/vaccinations/
Click here to read a copy of 'Should I Get a Vaccine'.
Click here to book your Covid-19 Vaccine

- MY PERSONALISED CARE PLAN
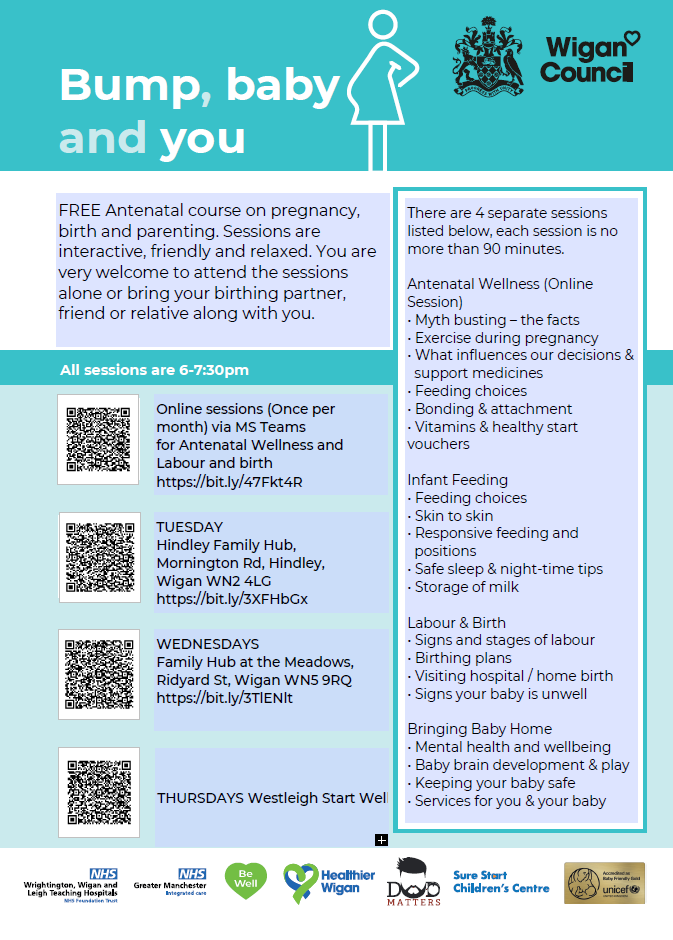
- PARENT EDUCATION
Infant Feeding and Skin to Skin
https://www.wwl.nhs.uk/our-departments?service=111
Further Resources
https://healthierwigan.nhs.uk/my-support/start-well/pregnancy/#1579813348437-111ad16a-37a7
- YOUR BABYS MOVEMENTS
Please follow the link below for information on your baby’s movements during pregnancy:
https://www.tommys.org/pregnancy-information/pregnancy-symptom-checker/baby-fetal-movements
If you have concerns about your baby’s movements, please phone our Maternity Triage on 01942 778628 we are open 24 hours a day seven days a week.
An information leaflet is available via the link below in English and other languages:
- INFORMATION LEAFLETS
Please click here to go to the Maternity patient information leaflet section.
- EARLY PREGNANCY ASSESSMENT UNIT
During the normal working week all women with early pregnancy problems such as pain or bleeding have prompt access to a dedicated Early Pregnancy Assessment Unit (EPAU) located at Ward 2 in Leigh Infirmary and open between 9am to 12noon.
You can self-refer to the service on 01942 264252 or 01942 264256.